Endoscopic Discectomy vs. Microdiscectomy
Back and leg pain from a herniated disc can change how you move through the day. Sitting hurts, standing too long hurts, and sleep gets interrupted. When imaging shows that a disc is pressing on a nerve and conservative care has not brought relief, surgery may become part of the conversation.
Two options often discussed are endoscopic discectomy and microdiscectomy. Both relieve nerve pressure from a herniated disc differently.
What Is an Endoscopic Discectomy?
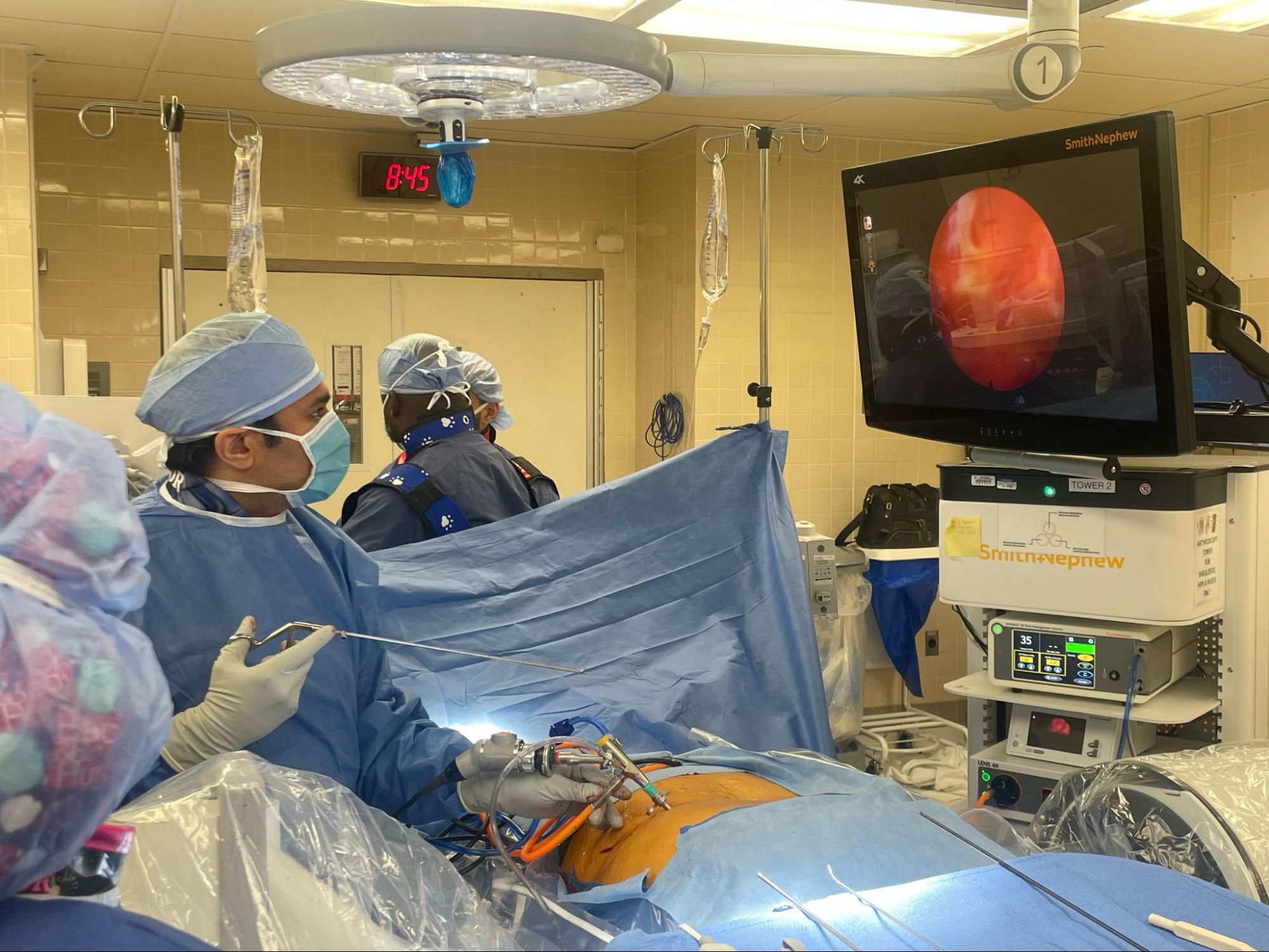
An endoscopic discectomy is a minimally invasive way to treat a herniated disc. The surgeon uses an endoscope, a small camera, through a small incision to see the problem area and guide precise instruments to the disc. Instead of wide exposure, the work stays focused on the compressed nerve. The aim is simple: remove the disc fragment causing irritation while keeping surrounding muscle and tissue disruption low.
When Is It Used?
Endoscopic discectomy is most often used for a single-level lumbar disc herniation that causes leg pain, numbness or weakness. It is typically considered after non-surgical care, such as physical therapy or when injections have not provided enough relief.
It may not be the right choice for every disc problem. Multi-level disease or certain anatomical patterns can make other approaches more appropriate. Your surgeon looks closely at imaging and symptoms before recommending this option.
Benefits
The appeal of endoscopic techniques comes from how targeted they are.
- Smaller incisions and less muscle disruption
- Minimal blood loss during surgery
- Often performed as an outpatient procedure
- Less postoperative pain for many patients
Some studies comparing endoscopic discectomy vs. microdiscectomy show similar long-term outcomes, with endoscopic approaches sometimes linked to less back pain in the first few months after surgery. Early recovery can feel smoother for certain patients, especially those eager to return to light activity sooner.
Potential Drawbacks
Endoscopic discectomy is not suitable for every patient. Surgeon experience also matters because the technique has a learning curve. In the wrong clinical situation, it may not provide enough access to fully decompress the nerve. At University Orthopaedic Associates, our spine surgeons possess the specialized training and experience necessary to determine the exact clinical situations where this approach will be most effective.
By choosing a team that excels in endoscopic techniques, you benefit from lower complication rates for issues like fluid leaks or nerve irritation, ensuring a safer path to recovery.
What Is a Microdiscectomy?
A microdiscectomy is one of the most performed surgeries for herniated discs. It removes the portion of disc pressing on the nerve using magnification and small instruments. Sometimes, a small amount of bone is also removed to improve access.
When Is It Used?
Microdiscectomy is typically recommended when leg or arm pain from a disc herniation does not improve after several weeks of conservative treatment. It may also be advised sooner if there is progressive weakness or trouble walking.
Urgent surgery is considered when symptoms involve bowel or bladder changes, which can signal a more serious nerve condition.
Benefits
Microdiscectomy is well studied and widely practiced.
- Strong relief of leg pain in properly selected patients
- Clear and direct access to the compressed nerve
- Predictable surgical steps with long-term data
Many people return to daily activities within a few weeks, with lifting restrictions easing over time.
Potential Drawbacks
Microdiscectomy can be effective, but you still weigh benefits against potential drawbacks. Most people follow temporary restrictions while healing. Possible complications include infection, bleeding, nerve irritation or a spinal fluid leak.
Studies report recurrent herniation in roughly 5 to 15 percent of cases, which can mean repeat surgery. A smaller group also reports lingering back discomfort.
How Outcomes Compare
When comparing endoscopic discectomy with microdiscectomy, research often shows more similarities than differences. Both approaches can effectively relieve nerve pain when used for the right patient.
Endoscopic techniques may provide benefits in facilitating early recovery and preserving soft tissue. Microdiscectomy is well-known and can be used on many different types of discs. Neither approach is universally better.
Finding the Right Surgical Path
Deciding between endoscopic discectomy and microdiscectomy is rarely a simple checkbox decision. It depends on how your disc herniation looks on imaging, which nerve is involved, and how long symptoms have been affecting your daily life. Pain patterns matter. So does whether weakness, numbness or activity limits are getting worse over time. Your overall health and the kind of movement you hope to return to also factor into the discussion.
At University Orthopaedic Associates (UOA), we take time to review these details together. We look closely at imaging, correlate it with your exam and talk through why one approach may offer better access, recovery expectations or long-term relief in your specific situation. No two spines behave the same, and treatment plans should reflect that reality. To learn more, the most important step is a one-on-one conversation.
Start the Conversation
If disc-related pain continues despite conservative care, a focused surgical evaluation can bring clarity. Schedule a consultation with our spine team to discuss whether endoscopic discectomy or microdiscectomy fits your anatomy, symptoms and goals.