What Is Ankle Arthritis?
Ankle arthritis occurs when the smooth cartilage that protects the bones in the ankle is slowly worn down. As that protective layer becomes thinner, the bones begin to rub directly against one another. Over the course of time, this can cause pain, swelling, stiffness, and structural changes to the joint that make mobility more of a challenge.
Ankle arthritis can occur in the talocrural joint, which is located between the tibia/fibula and talus, but can sometimes affect neighboring joints.
Types of Ankle Arthritis
There are three major types of ankle arthritis:
- Osteoarthritis (degenerative): The gradual “wear and tear” breakdown of cartilage
- Rheumatoid arthritis (inflammatory): An immune-mediated joint destruction
- Post-traumatic arthritis: Follows injury, such as fractures or ligament tears
In ankle cases, post-traumatic causes dominate, with 80% of ankle osteoarthritis linked to previous trauma. Knee and hip arthritis are 10x times more common than ankle arthritis.
Causes of Ankle Arthritis
Your ankle endures stress with every step. Because many people injure their ankles early in life, arthritis may appear decades later.
Arthritis can arise from the following:
- A past fracture (especially malleolar) or severe ankle sprain
- Misalignment after injury (even 1 mm of shift can drop the contact area by ~40%)
- Chronic ligament instability leading to abnormal wear
- Inflammatory disease, such as rheumatoid arthritis
- Congenital or structural deformities
Ankle Arthritis Symptoms
Signs and symptoms often build over time. What begins as mild discomfort after long walks can, over months or years, lead to daily pain, stiffness, and fatigue that affect both movement and mood.
Common symptoms include:
- Dull or sharp pain with walking or standing
- Morning stiffness or “gelling” after rest
- Swelling around the joint, warmth, tenderness
- Grinding, catching, or “bone on bone” sensation
- Limited motion, especially dorsiflexion/plantarflexion
- Weakness, instability, altered gait
How Ankle Arthritis Is Diagnosed
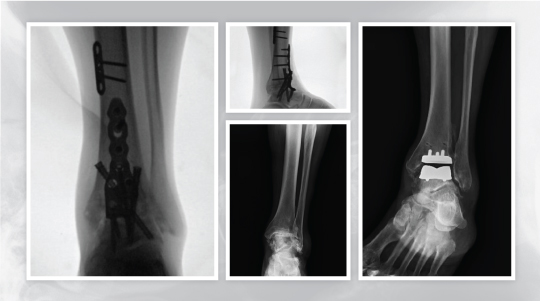
Imaging assists in staging the disease and implementing treatment options, that is, identifying bone deformities, osteochondral lesions, and joint malalignment.
Your physician will start with:
- History, such as when it began, the progression, or any past injury
- Exam: range of motion, swelling, palpation, alignment
- Weight-bearing X-rays to evaluate joint space loss, osteophytes, and subchondral sclerosis
- CT or MRI as needed to evaluate bone alignment, cartilage, and soft tissue
Ankle Arthritis Treatment
At University Orthopaedic Associates (UOA), we aim to ease your symptoms, protect joint function, and delay invasive surgery when possible.
Non-surgical options
- Activity modification (avoiding high-impact activities)
- NSAIDs, analgesics, anti-inflammatories
- Orthotic or brace ankle-foot orthosis to stabilize and offload weight
- Physical therapy, including strength training, flexibility training, and gait training
- Corticosteroid injection for short-term swelling relief
Surgical Options
If conservative care no longer eases your pain, your specialist may recommend surgery to restore comfort and function. One option is arthroscopic debridement, a minimally invasive procedure that removes inflamed tissue or bone spurs from the ankle joint. This approach can reduce stiffness and improve mobility in the early stages of arthritis.
For more advanced damage, ankle arthrodesis, also known as fusion, joins the bones of the ankle into a single, stable unit. By stopping motion in the worn joint, fusion helps relieve chronic pain and allows you to bear weight more comfortably. It remains one of the most reliable solutions for long-term relief.
Another option is total ankle replacement (TAR), where the damaged joint surfaces are replaced with a prosthetic implant. This technique preserves motion while addressing pain caused by severe arthritis. Ideal candidates have healthy bone quality, good circulation, and stable alignment.
Your UOA surgeon will guide you through each choice, explaining benefits, recovery time, and how each procedure fits your lifestyle and activity goals.
Recovery and Outlook
Outcomes depend on procedure and patient factors. Fusion reliably alleviates pain and yields high patient satisfaction, especially in younger, non-diabetic patients. However, fusion eliminates motion and may accelerate arthritis in nearby joints over time.
TAR preserves motion, and many patients return to moderate activity. But implants may loosen or fail, especially under high demand. In revision TAR cases, many failures convert to fusion. Your overall prognosis improves with adherence to rehab, weight management, and avoiding undue joint stress.
Request an Appointment With Our Foot and Ankle Specialists
Are you armed with symptoms or imaging results, or are you just seeking expert evaluation? At UOA, we combine data, advanced imaging, and hands-on experience to develop the right care plan for you.
Visit our Foot & Ankle Services page to learn more about UOA’s treatment options, or reach out and schedule an appointment. Let our specialists help you take confident steps toward better mobility.